Guide to End Stage Renal Disease (Kidney Failure)
On Page Nav:
Reviewed by the physicians of Columbia’s Kidney Transplant Team (December, 2023)
Each year more than 50,000 people in the United States are diagnosed with end-stage renal disease (ESRD).
End-stage renal disease occurs when approximately 90% of normal kidney function has been lost. Symptoms include nausea, vomiting, weakness, fatigue and sluggishness, confusion and difficulty concentrating, decreased urine output, anemia, and loss of appetite. It can cause complications such as high blood pressure and congestive heart failure (a buildup of fluid in the heart).
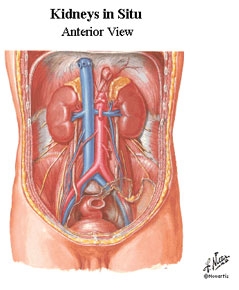
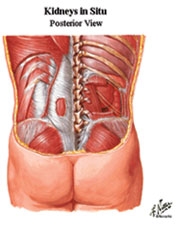
The Kidneys and How They Function
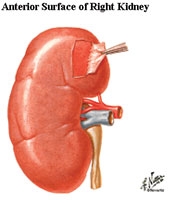 The kidneys, two bean-shaped organs located on either side of the spine at the level of the lowest ribs, serve a variety of vital functions. At the junction of the circulatory and urinary systems, the kidneys' primary function is the removal of excess fluid and waste material from the bloodstream, beginning the process of eliminating them from the body as urine flowing through the ureters, into the bladder and, finally, exiting through the urethra. The kidneys also regulate the body's levels of sodium, potassium, calcium, and other chemicals which can become toxic if left to build up. In addition, the kidneys function as glands, producing hormones to help maintain normal blood pressure, enable the production of red blood cells, and aid the formation of bone.
The kidneys, two bean-shaped organs located on either side of the spine at the level of the lowest ribs, serve a variety of vital functions. At the junction of the circulatory and urinary systems, the kidneys' primary function is the removal of excess fluid and waste material from the bloodstream, beginning the process of eliminating them from the body as urine flowing through the ureters, into the bladder and, finally, exiting through the urethra. The kidneys also regulate the body's levels of sodium, potassium, calcium, and other chemicals which can become toxic if left to build up. In addition, the kidneys function as glands, producing hormones to help maintain normal blood pressure, enable the production of red blood cells, and aid the formation of bone.
 The kidneys have a remarkable operating capacity—a single kidney, working at just 20% of its capacity, can still provide all needed renal filtration and regulation. And, the kidneys are capable of altering their activities from day to day, constantly adjusting to the variety and amounts of foods and liquids that are consumed. As we fast one day, or overindulge the next, the kidneys compensate to keep the body's tissues from bloating with fluids or dehydrating.
The kidneys have a remarkable operating capacity—a single kidney, working at just 20% of its capacity, can still provide all needed renal filtration and regulation. And, the kidneys are capable of altering their activities from day to day, constantly adjusting to the variety and amounts of foods and liquids that are consumed. As we fast one day, or overindulge the next, the kidneys compensate to keep the body's tissues from bloating with fluids or dehydrating.
Through a network of millions of nephrons in each kidney, blood entering from the renal arteries is filtered, and through complex biochemistry, substances not required by the body (typically urea, creatinine and ureic acid) are removed, and others, such as blood cells, proteins, and some amount of water, are reabsorbed. Thus, the blood that leaves the kidney through the renal veins contains necessary salts, protein, sugar, calcium and other vital substances in the right proportion, while excess chemicals, toxins and fluids are sloughed off into the urinary tract.
Congenital anomalies, inherited disorders, injury, hypertension, exposure to toxins, kidney stones, tumors, and even infections in other parts of the body can result in compromised renal function. Many kidney diseases have no noticeable symptoms until substantial and irreparable damage has been done. When the kidneys can no longer function well enough on their own—termed "end-state renal disease" or ESRD—hemodialysis or peritoneal dialysis will be required to help eliminate waste and excess fluids from the blood. Dialysis cannot, however, replicate the kidneys' hormonal benefits. Transplantation has proven to be the one way to recover the quality of health, and quality of life, enjoyed before the onset of end-stage renal disease.
End Stage Renal Disease Treatments
There are two accepted treatments for ESRD:
- Dialysis, which substitutes for the kidneys in filtering body waste, and
- Transplantation, in which a failed kidney is replaced with a healthy donor kidney. For eligible patients, kidney transplantation offers freedom from dependence on dialysis machines, and breakthroughs in surgical techniques and immunosuppresion therapy afford this opportunity to more people than ever before. Kidney transplant recipients today can expect to lead normal, productive lives for decades. Also, kidney transplantation has been show to result in a longer life expectancy than dialysis.
Diseases of the Kidneys
 The most common causes of kidney failure that necessitate kidney transplantation include:
The most common causes of kidney failure that necessitate kidney transplantation include:
- Diabetes, whether Type 1 (juvenile) or Type 2 (adult-onset), is the leading cause of kidney failure in the U.S. Diabetes may cause many other diseases and complications, and should be monitored carefully. Naomi Berrie Diabetes Center
- High Blood Pressure and other vascular diseases.
- Autoimmune diseases such as chronic glomerulonephritis and lupus, which cause chronic inflammation of the kidneys.
- Congenital disorders such as obstructive uropathy (blockages in the urinary tract), which can cause irreversible kidney failure.
Other conditions resulting in end-stage renal disease may be
indications for renal transplantation:
- Pyelonephritis
- Polycystic kidney disease
- Congenital urinary tract defects
- Alport's disease
- Hypertensive nephrosclerosis
- Reflux neuropathy
- Interstitial nephritis
- IgA nephropathy
- Goodpasture's syndrome
- Hemolytic uremic syndrome
- Chemical nephrotoxicity
- Renal artery emboli
- Sickle cell nephropathy
Contraindications for Renal Transplantation
Absolute contraindications for adults and children include (but may not be limited to):
- Advanced cardiopulmonary disease
- Active malignancy with the exception of skin cancer
- Severe local or systemic infection
Deceased Donor Kidney Transplant
Patients with advanced kidney failure who do not have the option of a living donor transplant join the waiting list for a deceased donor. The majority of kidneys transplanted in the United States are from deceased donors. Unfortunately, over 60,000 Americans are currently on the waiting list for a deceased donor kidney, with many waiting up to seven years to receive an organ.
Kidneys from deceased donors have a 50/50 chance of maintaining their function for 10-20 years post-transplant. In contrast, a live donor kidney has a 50/50 chance of functioning over 20 years, while a kidney from a perfectly matched sibling donor last for 35 years on average. In addition, 50-60% of deceased donor kidneys are fully functional immediately upon transplantation, versus 97% of live donor organs.
In light of these and other health advantages associated with live donor transplants, the surgeons at NewYork-Presbyterian Hospital/Columbia University Medical Center (NewYork-Presbyterian/Columbia) try to exhaust all live donor alternatives, including paired kidney exchanges and incompatible donors, before relying upon a deceased donor. In 2003, approximately 25% of the kidneys transplanted at NewYork-Presbyterian/Columbia were from deceased donors. However, currently approximately 50% of our kidney transplants are from deceased donors.
Transplant Procedure
Once a compatible organ has been identified and obtained, the surgeon places the kidney on one side of the recipient's front lower abdomen, using an 4-10 inch incision. The novel placement of the kidneys—versus its natural position at the back of the body—allows the surgeon to more easily connect the kidney to the bladder. To ensure an adequate blood supply, the surgeon also attaches the kidney to an artery and vein that lead to the legs. In most cases, the patient's own kidneys are not removed, thereby avoiding unnecessary additional surgery.
The transplant operation typically lasts from 2½-5 hours. The patient stays in the hospital for as little as three days and spends approximately six weeks recuperating at home. All organ transplant recipients, including kidney recipients, need to take daily immunosuppressant medications.
Next Steps
If you have severe kidney disease, we can help. Call us at (212) 305-6469 to get started today, or sign up with one of our online forms: I Need A Transplant » | I Want to Donate My Kidney »

Related Topics
- Kidney Transplant Surgery
- Living Donor Kidney Transplants
- Kidney Autotransplant
- Pancreas Transplants
- Facts About Organ Donation
- Becoming a Kidney Donor
Related Resources
- Transplant Evaluation Questionnaire
- Living Donor Evaluation Questionnaire
- Your Kidney Transplant
- Follow-Up Visits After Kidney Transplant Surgery
- Resuming Life After Kidney Transplantation
- Organ Rejection after Kidney Transplant
- Nutrition After Kidney Transplant
- Immunosuppressant Medications
- Infection After Kidney Transplant
This content has been created by Columbia’s Health Guide Team. Learn more about our efforts to bring you the clearest, most accurate, and most human health resources available.
