Guide to Congenital Heart Diseases
Congenital heart disease is a general term for any defect or malformation of the heart at birth. These diseases can range from mild with no symptoms to severe and life-threatening. About one in every 100 babies in the U.S. is born with a congenital heart disease, making it the most common type of birth defect.
Key Facts
- The word congenital means present from birth. The heart completely forms during the first eight weeks of gestation. Any abnormal development during this time will result in a congenital heart condition.
- While the exact causes of these defects are unknown, certain environmental and genetic risk factors appear most likely to play a role. A variety of diagnostic methods and tests are used to detect these abnormalities prior to birth.
- Most congenital heart defects do not require immediate treatment. However, about one in four involve a severe malformation, such as a missing or poorly formed structure, that will usually require surgery or another procedure within the baby’s first year.
Causes
Researchers are still studying what causes congenital heart disease. In some cases, there is a family history of congenital heart defects, which would suggest a genetic cause. Certain defects have also been linked to specific medications and maternal diseases. However, in most cases, no clear cause can be identified.
Risk factors linked to congenital heart disease include:
- Alcohol: Drinking alcohol during pregnancy has been linked to a higher incidence of heart defects in babies.
- Diabetes: While there is no known link between congenital heart disease and gestational diabetes, having type 1 or type 2 diabetes while pregnant may increase the risk of a heart defect.
- Genetics: If a parent has a congenital heart disease, their children are about three times more likely to also have one. This suggests that some heart defects may have a strong inherited cause.
- Medications: Several medications, when taken during pregnancy, have been linked to congenital heart disease. These include antiseizure drugs, lithium, and isotretinoin, which is used to treat acne.
- Rubella: Contracting rubella (also known as German measles) during pregnancy may cause heart defects in the developing fetus.
- Smoking: Smoking while pregnant has been linked to congenital heart disease.
Types
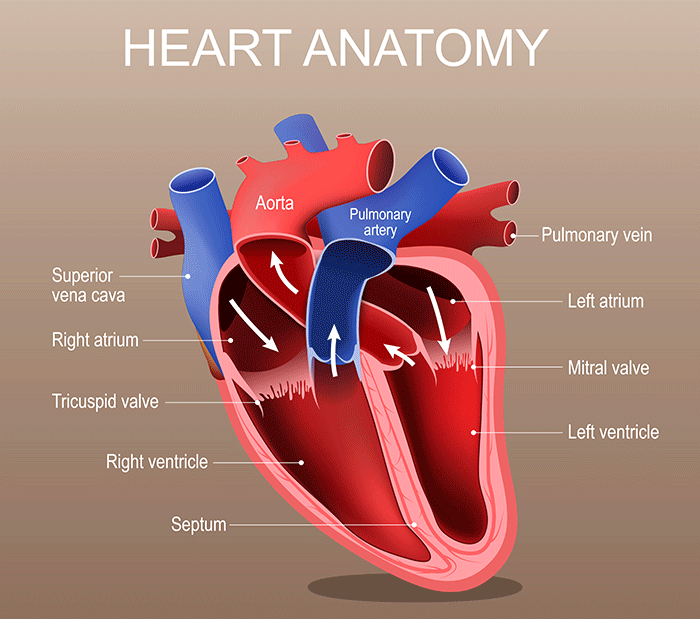
In order to understand the different types of congenital heart disease, it can help to first have a basic understanding of the structure, or anatomy, of the heart.
The heart is divided into four chambers: two on the top (the right and left atria) and two on the bottom (the right and left ventricles). The left and right sides of the heart are separated by a wall called the septum. Blood travels to each of these chambers through valves, which open and shut like doors. Large blood vessels carry blood into and out of the heart: The aorta carries oxygen-rich blood from the left side of the heart to the rest of the body, and the pulmonary artery carries oxygen-poor blood from the right side of the heart to the lungs. These parts all work together to keep blood circulating throughout the body.
Congenital heart disease is a defect in one or more of these part, and it can fall into three major categories:
Obstructive Defects
These kinds of defects are caused by underdeveloped valves between the chambers of the heart, which can make it difficult for the heart to pump enough blood to the body. They include:
- Aortic stenosis: The aortic valve does not form properly and is narrowed, restricting the amount of blood that can flow from the left ventricle to the aorta.
- Pulmonary stenosis: The pulmonary valve does not form properly and is narrowed, restricting the amount of blood that can flow from the lower right chamber to the pulmonary arteries.
- Coarctation of the aorta: A narrowing of the aorta, the largest and most vital blood vessel in the body. This restricts blood flow from the heart to the rest of the body.
Septal Defects
Septal defects allow blood to pass between chambers of the heart due to an opening in the wall, or septum, separating them. This can lead to congestion and other complications. These defects include:
- Atrial septal defect (ASD): An opening between the right and left atria, leading to abnormal blood flow.
- Ventricular septal defect (VSD): An opening between the right and left ventricles. Blood pressure is higher in the left ventricle, so more blood flows into the right ventricle, leading to extra blood in the lungs.
- Atrioventricular septal defect (AVSD): An opening in the septum that separates the two atria (upper chambers) and the two ventricles (lower chambers). In a Complete AVSD, a single large hole can open into all four chambers. AVSD is sometimes referred to as an AV canal.
Cyanotic Defects
These defects restrict blood flow to the lungs, making it more difficult for enough oxygen to circulate through the body. This can lead to cyanotic (blue-tinged) skin, difficulty breathing, and poor weight gain, among other complications. Types of cyanotic congenital heart disease include:
- Tetralogy of Fallot: A combination of four different defects that result in an abnormal flow of blood from the heart to the body. It is the most common cyanotic defect:
- A hole between the left and right ventricles (ventricular septal defect)
- A narrow pulmonary artery (pulmonary valve stenosis)
- A thickening of the right ventricle (right ventricular hypertrophy)
- A misaligned aorta (overriding aorta)
- Transposition of the great arteries: This is a rare but serious defect in which the two main arteries, the aorta and pulmonary artery, are switched. This causes oxygen-poor blood to be pumped out to the body and oxygen-rich blood to be returned back to the lungs. This condition requires immediate treatment.
Symptoms
Symptoms vary depending on the type of congenital heart disease. Some types may have very few or even no symptoms, while others may have significant and severe complications. Still others may only present symptoms later in life.
General symptoms common to most forms of congenital heart disease include:
- Blue skin, lips, or fingernails (cyanosis)
- Difficulty breathing
- Irregular heart rhythms (arrhythmias)
- Persistent fatigue
- Swelling due to excess fluid (edema)
Explore our condition page for each congenital heart disease to learn about their specific symptoms.
Diagnosis
Congenital heart disease is often diagnosed during pregnancy. However, milder heart defects may not be detected until after a baby is born.
During Pregnancy
Congenital heart disease may first be suspected during a routine prenatal ultrasound. To confirm the diagnosis, a specialized ultrasound called a fetal echocardiogram is used to create a detailed image of the fetus’s heart. This test is typically carried out during the second trimester of pregnancy. There are two ways to perform a fetal echocardiogram:
- Abdominal ultrasound: A gel is applied to the mother’s abdomen, then an ultrasound probe is placed on top and moved around to create an image of the fetus’s heart. This is the most common method.
- Endovaginal ultrasound: A small probe is inserted into the mother’s vagina, providing more detailed images of the fetus’s heart. This test can be performed earlier in the pregnancy than the abdominal ultrasound.
After Birth
If a diagnosis is not made before birth, it may be possible to make a diagnosis shortly after birth. The baby may show symptoms of congenital heart disease, such as cyanosis (blue skin, lips, or fingernails) or a heart murmur, during a routine newborn physical exam. This involves the doctor taking the baby’s pulse and listening to their heart using a stethoscope.
Sometimes signs of congenital heart disease will not appear until later in life. When this is the case, other tests may be used to make a diagnosis, including:
- Cardiac catheterization: This procedure is used to gain vital information about how various parts of the heart are functioning. It involves inserting a thin, flexible tube called a catheter into a blood vessel and up into the heart so different measurements can be taken.
- Chest X-ray: This test creates a detailed picture of the heart and lungs, allowing doctors to check for signs of disease.
- Echocardiogram: This technique uses sound waves to produce an image of the heart. Doctors can use it to see the heart beating and pumping blood while they look for defects.
- Electrocardiogram: This test measures the electrical activity of the heart. Sensors called electrodes are attached to the patient’s arms, legs, and chest to measure how well the heart is beating.
- Pulse oximetry: This simple, noninvasive test measures oxygen levels in the blood. A small sensor is placed on the fingertip to track how well light waves are absorbed. This information is then used to determine how much oxygen is present.
Treatment
Treatment for congenital heart disease will depend on the specific type of defect. In many cases, no treatment will be necessary. Instead, regular monitoring will be required to ensure the heart is functioning properly.
For more severe cases, surgery is the most common form of treatment. Whenever possible, minimally invasive procedures such as catheterization may be used. This involves inserting a catheter into an artery to guide instruments up into the heart to repair defects or improve blood flow.
Occasionally, medications are used to relieve symptoms. These may include diuretics to remove excess fluid or drugs that slow down the heart and increase strength, such as digoxin.
Explore our condition page for each congenital heart disease to learn about their specific symptoms.
Outlook
The survival rate of babies with congenital heart disease depends on several factors, such as the type of defect, when it is diagnosed, and how it is treated. However, advances in diagnostics and treatments have helped increase the rate of survival over the past several decades.
According to CDC statistics, the survival rates for congenital heart disease are:
Non-critical congenital heart disease survival rates
- 97% survive to at least 1 year old
- 95% survive to at least 18 years old
Critical congenital heart disease survival rates
- 75% survive to at least 1 year old
- 69% survive to at least 18 years old
Next Steps
If your child has a congenital heart disease, the Congenital Heart Center can help. Our team can offer personalized treatment plans delivered with a level of quality that could only come from one of the most experienced programs in the country.
Call us at 212-305-2688 or use our online form to schedule an appointment.
