Guide to Barrett's Esophagus
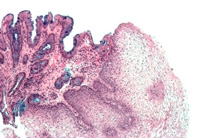 Barrett’s esophagus is a condition in which repeated contact with gastric acid (gastroesophageal reflux, or GERD) transforms a patient’s esophageal cells from normal squamous epithelium to abnormal intestinalized columnar epithelium. Barrett’s esophagus greatly increases the risk of developing esophageal cancer.
Barrett’s esophagus is a condition in which repeated contact with gastric acid (gastroesophageal reflux, or GERD) transforms a patient’s esophageal cells from normal squamous epithelium to abnormal intestinalized columnar epithelium. Barrett’s esophagus greatly increases the risk of developing esophageal cancer.
Risk Factors
Risk factors for Barrett’s esophagus include chronic, long-lasting gastroesophageal reflux, obesity, and smoking.
Diagnosis
Barrett’s esophagus is diagnosed with upper GI endoscopy and biopsy. Our endoscopists use the latest technology for the minute inspection of abnormal areas in the esophagus, including a modified blue light examination called narrowband imaging (NBI) for patients with Barrett's esophagus. In conjunction with high resolution video endoscopes and electronic magnification, remarkably detailed views of the surface lining of Barrett's esophagus can be obtained to direct precision biopsies and guide therapy.
Capsule endoscopy, which has been shown to be effective in diagnosing conditions of the small intestine, is being evaluated as a non-invasive alternative for diagnosing Barrett's esophagus.
Digestive disease specialists at NewYork-Presbyterian/Columbia offer promising techniques for the diagnosis of Barrett's esophagus and continue to examine the benefits of screening for adenocarcinoma in patients with Barrett's to prevent the development of cancer.
Treatments
Treatments for Barrett’s esophagus include; medications, endoscopic ablation therapies, endoscopic mucosal resection, and surgery.
Ablation Therapy
 Endoscopists at Columbia use BARRX HALO technology, an advanced form of ablation that delivers heat energy in a precise and highly-controlled manner. This catheter delivers a short burst of radiofrequency energy circumferentially to the esophagus, which eliminates the abnormal Barrett’s epithelium and allows the normal squamous epithelium to regrow. It is capable of achieving complete removal of the dysplastic Barrett’s epithelium without damage to the normal underlying structures.
Endoscopists at Columbia use BARRX HALO technology, an advanced form of ablation that delivers heat energy in a precise and highly-controlled manner. This catheter delivers a short burst of radiofrequency energy circumferentially to the esophagus, which eliminates the abnormal Barrett’s epithelium and allows the normal squamous epithelium to regrow. It is capable of achieving complete removal of the dysplastic Barrett’s epithelium without damage to the normal underlying structures.
Our physicians are actively testing combining of radiofrequency ablation with acid suppression so a normal lining grows back with healing. Early results are highly promising, showing high efficacy for complete removal of Barrett's esophagus with a very low incidence of serious side effects. Efficacy and safety appear clearly improved compared with prior laser-based ablation therapies.
Endoscopic Mucosal Resection
Patients with Barrett's esophagus who develop a small focus of cancer can often be spared a radical surgical procedure by opting instead for endoscopic mucosal resection (EMR).
Performed through the endoscope, EMR involves injection of a solution under the abnormal area of the esophagus. Suction is then applied to create a small polyp of tissue, and a snare is used to resect the area, much like the process of removing a colon polyp. While this procedure cannot remove tissue from the entire circumference of the esophagus, EMR can be used to remove a small superficial cancer or a localized area of high-grade dysplasia.
Endoscopic ultrasound (EUS) is used to judge whether EMR is appropriate and is also effective for staging, providing definitive evidence on the depth of the tumor.
Next Steps
If you are in need of help for an esophageal condition, we’re here for you. Call us now at (212) 305-1909 or fill out our online form to get started today.
Related Topics
- Achalasia
- Barrett's esophagus
- Esophageal atresia
- Esophageal cancer
- Esophageal dilation
- Esophagectomy
- Gastroesophageal reflux disorder (GERD)
- Hiatal hernia
- Swallowing disorders/dysphagia
This content has been created by Columbia’s Health Guide Team. Learn more about our efforts to bring you the clearest, most accurate, and most human health resources available.
