A new study from the Global Center for Integrated Colorectal Surgery and IBD Interventional Endoscopy supports the use of this complex but effective procedure, pointing to high patient satisfaction and improved quality of life.
For people with chronic digestive conditions like ulcerative colitis, a top priority for surgery is avoiding an external ostomy bag. While the current solution, the ileal pouch-anal anastomosis, or J-pouch procedure, is an effective option for many patients, new research suggests that another, older surgery may be a viable alternative: the continent ileostomy, or K-pouch.
Ravi P. Kiran, MD, Co-Director of the Global Center for Integrated Colorectal Surgery and IBD Interventional Endoscopy at NewYork-Presbyterian and Columbia University Irving Medical Center, recently published a decade-long retrospective study that highlights the K-pouch procedure’s durability, safety, and high levels of patient satisfaction.
“There are many advantages to the K-pouch,” says Dr. Kiran. “We have seen very good outcomes for patients. They report a good quality of life.”
Avoiding an Ostomy Bag
The removal of the entire colon requires a new long-term solution for waste removal. For decades, standard treatment was an end ileostomy: the end of the small intestine is brought through an opening in the abdomen, creating a permanent opening (stoma). This procedure requires a person to wear an external ostomy bag to collect any waste that passes through the stoma.
The external bag presents several practical challenges and has been shown to have a significant negative impact on quality of life. Modern surgeons have focused on solutions that avoid the need for an ostomy bag.
The most popular solution is the ileal pouch-anal anastomosis (IPAA or J-pouch), a surgical technique that creates a J-shaped internal reservoir out of the small intestine, which is then connected to the anus. This allows the patient to have bowel movements similar to what they are accustomed to, avoiding the need for an external ostomy bag.
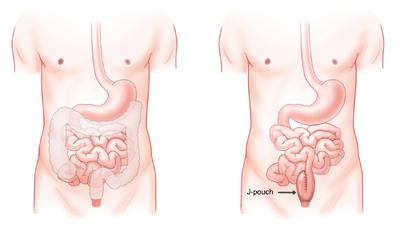
But for patients with failed J-pouch surgeries or those lacking the necessary anatomy for a successful J-pouch, Kiran advocates for an effective alternative: the continent ileostomy (CI), also known as the K-pouch (Kock pouch).
Looking at the K-Pouch in a New Light
Named after Dr. Nils Kock, the K-pouch procedure was originally created in 1967 to address an issue associated with the end ileostomy: the uncontrolled passing of stool through the stoma (opening) into the external ostomy bag.
With a K-pouch, an internal reservoir is created out of the small intestine and attached to a stoma in the abdomen.
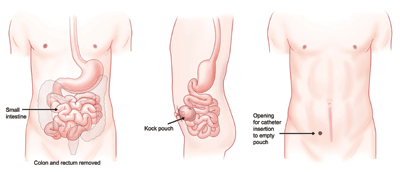
Stool can then be removed by the patient using a catheter. Unlike an end ileostomy, a K-pouch does not require an external ostomy bag. Patients remove their waste using a catheter inserted into the stoma.
K-Pouch Vs J-Pouch: What’s the Difference?
J-Pouch (Ileal Pouch–Anal Anastomosis, IPAA)
- A surgical procedure that creates an internal J-shaped pouch from the small intestine.
- The pouch is directly connected to the anus, allowing patients to pass stool naturally (without the need for a permanent ostomy bag).
- Most often used for ulcerative colitis or familial adenomatous polyposis after removal of the colon and rectum.
K-Pouch (Continent Ileostomy, Kock Pouch)
- A surgically created internal reservoir made from the small intestine.
- Instead of connecting to the anus, the pouch connects to the abdominal wall with a small stoma and valve system.
- Patients empty the pouch by inserting a catheter through the small external opening (usually 3–5 times per day).
- Often used when a J-pouch is not possible or has failed, or for patients who cannot manage a traditional ostomy bag.
The K-pouch fell out of favor in part because of its technical complexity; it is a complicated surgery that requires a highly skilled surgeon. It also has a learning curve that can be intimidating to patients, as it requires regular emptying of the reservoir using a catheter, which is typically done three to five times a day.
But Dr. Kiran and his colleagues argue that the benefits of the K-pouch often outweigh the challenges. “It can improve cosmetic appearance, allow for better activity and exercise, address skin problems, and potentially improve nutrient absorption compared to standard end ileostomies.
Who is a Candidate for K-Pouch Surgery?
Ideal candidates for K-pouch include patients with:
- J-pouch failure
- Low tolerance for external ostomy appliances
- Skin issues near the stoma
- Pelvic floor dysfunction or impaired continence
Requirements include:
- Adequate small bowel length and healthy bowel tissue
- Approximately 60 centimeters of small intestine is needed to create the pouch and valve.
Result of the Study
The study examined the outcomes from 95 K-pouch procedures performed on 80 patients from 2013 to 2023, including:
- 38 new pouch creations
- 52 revisions
- 5 pouch excisions
The results were encouraging. After an average of three years of follow-up:
- 87% of patients retained their K-pouch
- Pouch revision was required in 34% of patients
- 92% of patients in the new pouch group and 93% in the revision group reported improvements in function and quality of life
- 96% stated they would recommend the procedure to others.
“If you look at their quality of life and happiness, the data supports that the K-pouch is a good option to offer to patients,” says Dr. Kiran.
For complex IBD patients facing life-altering decisions (whether from their disease or the failure of previous surgeries), there is a clear need for alternative solutions that avoid an ostomy bag. The K-Pouch offers a viable and practical option that many simply never hear about.
“Many providers simply don’t offer it because they’re not aware it exists or they don’t believe it works,” Dr. Kiran says. “But when done well, patients are overwhelmingly satisfied and grateful for the improved quality of life it offers.”
Dr. Kiran points to the study's results as a call for the continent ileostomy to receive renewed consideration among gastroenterologists and for increased awareness and training among colorectal surgeons.
“This surgery should not be a relic of the past,” Dr. Kiran says. “In the right hands, with the right support, the K-pouch is a forward-looking option for the right patient.”
Related
- I Need a… Colorectal Surgeon
- Dr. AI: Can I Live a Normal Life with a Colostomy Bag?
- What Is Interventional IBD ?

