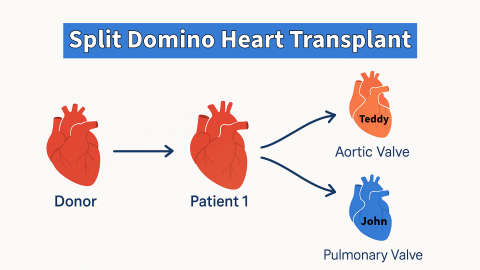
In a single, intense 24-hour period, pediatric heart surgeons at Columbia took on a surgical feat rarely performed—a split-domino heart transplant. It’s a surgery of cascading proportions where a donor's heart is transplanted into a child, and the healthy parts of that child’s explanted heart are used to save two additional lives.
Late in the summer of 2024, three children—a 10-year-old girl, John, and Teddy—were the first to receive a split-domino heart transplant in New York, each undergoing a different complex open-heart procedure in carefully orchestrated stages. Led by David Kalfa, MD, PhD, and Andrew Goldstone, MD, PhD, this timeline provides a glimpse into the choreography and precision that goes into a surgical operation comprised of three separate operations on three different children. Let’s dive in:
Operation 1: The Donor’s Heart Transplant
Operation 2: John’s Pulmonary Valve Replacement
Operation 3: Teddy’s Aortic Valve Replacement
Pre-Surgery Preparation: The Warm Up
Weeks of careful planning preceded the surgery. Each step was thought out: from accepting the donor heart for a 10-year-old girl suffering from idiopathic dilated cardiomyopathy (a condition where the heart's left ventricle becomes enlarged and weakened, making it harder for the heart to pump blood efficiently), to measuring valve diameters of the recipient children, John and Teddy, in anticipation of the pulmonary and aortic valve replacements.
The logistics for the domino transplant were intricate. Two operating rooms (ORs) were prepared, and Dr. Kalfa and Dr. Goldstone led separate teams using a staggered approach.
Timing was everything.
8:00 AM: Donor's Heart Transplant Begins
Their 10-year-old donor was the first to enter the OR. Living with an implanted mechanical pump for seven weeks, called the Berlin LVAD, that helps the heart's left ventricle pump blood to the rest of the body, her team got word that a new heart was coming. Dr. Kalfa began the complex task of explanting her failing heart while the donor’s heart was transported to the hospital.
Simultaneously, Dr. Goldstone began prepping John, the 18-month-old boy in the next room, who would receive her pulmonary valve.
10:30 AM: The Heart is Explanted
At around 10:30 AM, the surgical team confirmed that her donor heart was in excellent condition, and the heart explantation began. With the original heart removed, Dr. Kalfa carefully extracted the pulmonary valve and transferred it to Dr. Goldstone in the adjacent room.
While the pulmonary valve was prepared for John, their donor’s new heart was placed in a SherpaPak—a device designed to keep the organ at an optimal temperature while it awaited transplant.
11:00 AM: John's Pulmonary Valve Replacement Begins
Dr. Goldstone, now working with the freshly explanted pulmonary valve, started John’s surgery. Previously, John had a surgery called truncus arteriosus repair to correct a congenital heart defect where a single large blood vessel comes out of the heart instead of two separate ones. Now, he needed a new pulmonary valve, as his existing one had degenerated.
As John’s surgery progressed, his donor’s heart transplant continued in the OR next door, and both teams worked in parallel.
2:00 PM: Their Donor’s New Heart is Implanted
By mid-afternoon, John and Teddy’s donor had successfully received her donor heart. The next critical steps involved ensuring proper heart function, checking for complications, and coming off bypass.
At this time, Dr. Kalfa and his team began preparing the second room for Teddy, a three-year-old boy who would receive her aortic valve later in the evening. Teddy had experienced recurring aortic valve obstructions and needed a full valve replacement.
4:00 PM: John’s Surgery Finishes
By late afternoon, John’s pulmonary valve replacement was completed successfully, and he was stable. After a day of staggered operations, the teams prepared for the final phase of the domino transplant.
Dr. Kalfa was able to snag an hour of shut-eye here, too. Phew.
7:00 PM: Teddy’s Aortic Valve Replacement Begins
The third surgery began late in the evening. Teddy, who had already undergone a balloon valvuloplasty at three months old for aortic valve stenosis, a procedure where a small balloon is inserted and inflated to widen a narrowed heart valve and improve blood flow, was ready for his aortic valve transplant. Dr. Kalfa carefully detached the aortic valve from her explanted heart, which took about 20 minutes due to the complexity of the surrounding structures and her previous ventricular assist device (VAD).
2:00 AM: A Surprise Complication
A complication appeared during surgery when a surprise abnormality was uncovered in her heart—a previously undetected malformation of her coronary arteries. Their donor had a coronary artery that runs inside the heart muscle instead of on its surface. This required Dr. Kalfa to think fast. He performed what’s called an unroofing procedure. With this surgical technique, he removes part of the heart muscle that is "covering" the artery, allowing it to sit more normally on the heart's surface and improving blood flow. In those few darkest hours before dawn, the problem was repaired, and blood flow stabilized.
4:00 AM: Teddy's Surgery Finishes
As the early morning hours approached, Teddy’s aortic valve was successfully implanted, and the surgical team ensured that there were no complications with his coronary arteries or heart function. Teddy was stable and came off bypass smoothly. And with that, the final sequence of this surgical ballet's third act ended.
Post-Surgery: A Smooth Recovery
All three children had smooth postoperative recoveries. She was extubated one day after surgery and discharged 22 days later with no complications. John was also extubated the day after his surgery and discharged on post-op day nine. Teddy, despite the challenges faced during his surgery, was similarly extubated on day one and discharged home nine days later.
Eight months after the groundbreaking surgery, all three patients are doing exceptionally well—a testament to the careful planning, skill, and collaboration of the entire surgical team.
A Triumph of Surgical Precision and Teamwork
The domino transplant was a feat of surgical precision and team coordination, where three lives were saved through the thoughtful use of one donor heart. The ability to navigate multiple operations in parallel, adapt to unexpected complications, and deliver such outstanding outcomes stands as a testament to the pediatric heart surgery team’s relentless pursuit of the best possible heart care for children in New York and beyond.

