Guide to Intestinal Failure
Reviewed by the physicians of Columbia’s Intestinal & Multiorgan Transplant Surgery Team, March 2025
Intestinal failure is a condition in which people don’t have enough properly-working gut mass needed to meet their fluid and nutrient requirements. This can happen due to anatomical or functional loss of the gut surface area.
Key Facts
- Intestinal failure often occurs after a large piece of intestine is removed to treat other disease. This creates a condition called short bowel syndrome.
- People with intestinal failure may require a type of nutrition called TPN, which can lead to liver failure.
- Intestinal failure can be treated with a small bowel transplant (intestinal transplant)
What causes intestinal failure?
The most common causes of intestinal failure are short bowel syndrome (an issue that can occur if the intestine is damaged or shortened, often as a result of surgery) and liver failure associated with TPN (total parenteral nutrition - nutrition delivered via veins rather than the GI tract).
Intestinal failure can happen even without short bowel syndrome. For example, dysmotility disorders (intestinal pseudo-obstruction), malabsorption and congenital diseases can all lead to intestinal failure.
A more complete list of conditions that can cause intestinal failure include:
- Blocked or obstructed intestines (atresia)
- Crohn’s disease
- Desmoid tumor with intra-abdominal infiltration
- End stage liver disease (cirrhosis)
- Endocrine tumors
- Gardner's syndrome
- Gastroschisis
- Hirschsprung's disease
- Infiltrative diseases leading to intestinal failure (sarcoidosis or amyloidosis)
- Megacystis microcolon intestinal hypoperistalsis syndrome (MMIHS)
- Mesenteric venous thrombosis or arterial thrombosis
- Microvillus inclusion disease
- Multiple resections and explorations
- Necrotizing enterocolitis
- Severe cholestasis induced by total parental nutrition (TPN-IC)
- Short bowel syndrome
- Vascular abdominal trauma
- Volvulus
How is intestinal failure managed?
Patients with intestinal failure are unable to maintain caloric intake by mouth or with a tube going into the stomach or intestines. They are fed through a vein with a liquid formula known as total parenteral nutrition (TPN). “Parenteral” means that a route other than the digestive tract is used for nutrition.
TPN formulas contain protein, carbohydrates, fats, electrolytes, vitamins and minerals. They come in 2-3 liter bags, and most people get at least one bag per day. The bag is connected to an infusion pump and the entire system fits into a backpack that the patient can wear or keep nearby.
Can TPN cause problems?
While some patients do well on TPN, others suffer from complications, including:
- episodes of severe infection related to the catheter
- liver problems
- frequent episodes of severe dehydration
- complications related to venous access like vascular injury and venous thrombosis.
How is intestinal failure treated?
Patients with intestinal failure may be candidates for intestinal rehabilitation or intestinal transplantation.
Medical Treatments
Non-surgical approaches to treating intestinal failure includes:
- Central catheter management
- Treatment with Gattex
- TPN (Total Parenteral Nutrition) management to prevent liver injury
- Special short gut diet
- Optimization of antisecretory and antimotility agents
To find out more about pediatric medical management of intestinal failure, visit our Pediatric Intestinal Rehabilitation Program.
Surgical Treatments
There are several different types of intestinal and multiorgan transplantation procedures. Which one you receive will depend on the cause of your condition and any related complications.
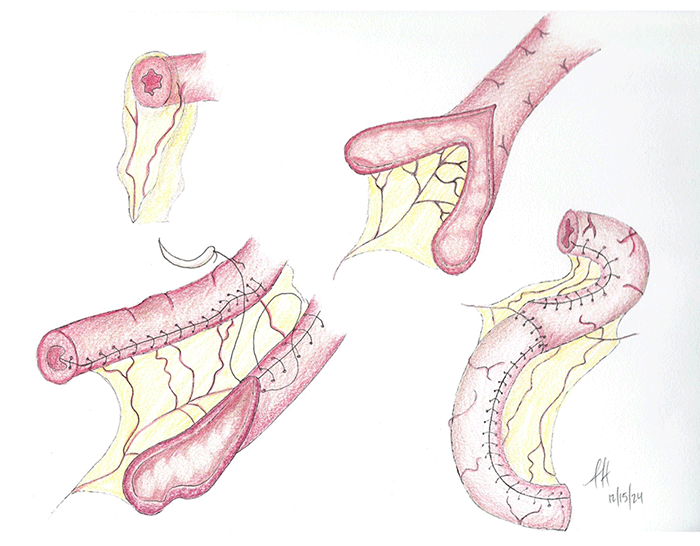
- Isolated Intestinal Transplant: Removes the diseased portion of the small intestine and replaces it with a healthy donor small intestine. This type of transplant is given to patients who have complications caused by intestinal failure, but do not have liver failure.
- Multivisceral Transplant: Removes multiple diseased organs and replaces them with healthy donor organs. This type of transplant is given to patients who have multiple organ failure, including stomach, pancreas, liver, small intestine, and/or kidney failure.
- Modified Multivisceral Transplant: Involves keeping your own liver while removing the remaining diseased organs and replacing them with healthy donor organs. This type of transplant is given to patients who do not have liver disease or failure, but do have organ failure of the stomach, pancreas, small intestine, and/or kidney.
- Ex Vivo Surgery: Removes as many as six abdominal organs in order to excise tumors that have grown around these organs and/or their blood vessels, and then reimplants these same organs back into the body.
Surgery for enterocutanous fistula
There are non-transplant surgical treatment options for enterocutaneous fistula, an abnormal connection between the intestines and the skin that can cause intestinal failure.
- Ostomy closure
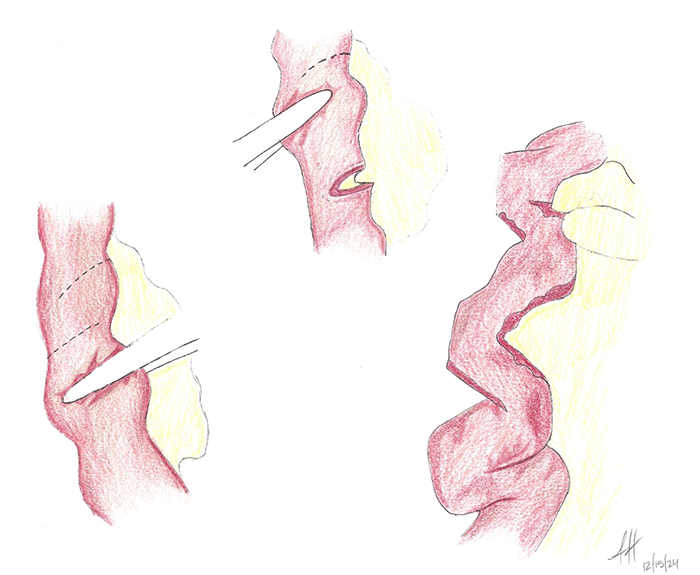
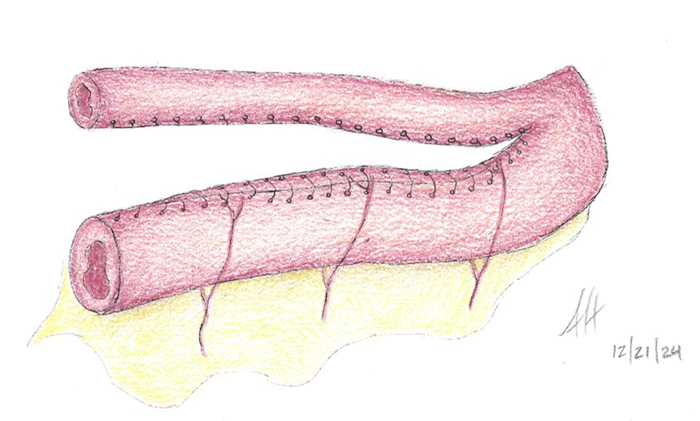
- Bowel lengthening procedure, such as the STEP (Serial Transverse Enteroplasty) procedure and the Bianchi procedure
- Bowel tapering
Learn more about intestinal & multivisceral transplantation and ex vivo surgery
When should patients be referred for a small bowel transplant evaluation?
It’s never too early, but it can be too late to refer a patient for a small bowel transplant evaluation. There is a high risk of death among patients waiting for intestinal transplants, so early referral of patients with risk factors is important.
Next Steps
If you or your loved one are dealing with intestinal failure, our Intestinal and Multiorgan Transplant Program can help. We are one of only a few transplant centers in the world to offer intestinal transplants and multiorgan transplants. Our team of dedicated specialists have over two decades’ worth of experience performing these complex procedures.
Call us at 877-548-3763 or use our online form to schedule an appointment.
Once you are referred to us, you will be evaluated by the surgical team, the medical team (gastroenterology, infectious disease, cardiology), social workers, and dietitians. A dedicated coordinator will shepherd you through the process. We will perform all of the necessary testing to ensure that we can treat you safely and effectively.
Related
- Read about our intestinal & multiorgan transplant program
- Learn about intestinal & multiorgan transplants
- Meet our transplant team
- Check out more resources
This content has been created by Columbia’s Health Guide Team. Learn more about our efforts to bring you the clearest, most accurate, and most human health resources available.
