A conversation with Tom O’Donnell, MD, vascular surgeon, about the innovations, reversals, and transformations shaping vascular surgery.
How would you describe the current state of vascular surgery, both in general and at Columbia?
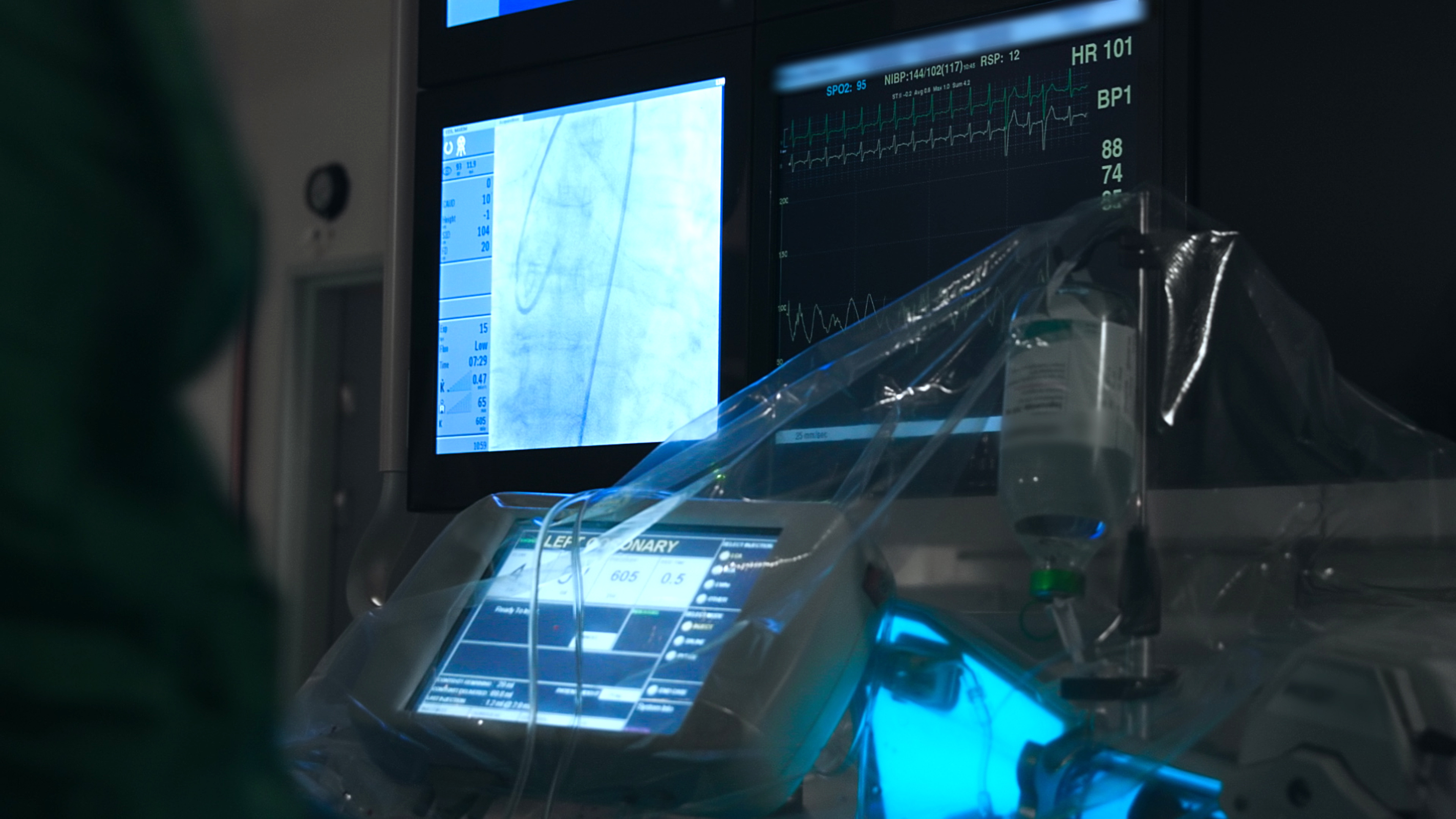
I think overall, we’re still in what’s been called the endovascular revolution. That’s the big shift over the last decade toward treating things like leg blockages or aneurysms in the belly or chest using catheters and stents rather than open surgery. That’s changed a lot in terms of patient recovery and outcomes.
But we’re also reaching a more balanced point now. There was this big swing toward endovascular, and now we’re starting to understand that for certain patients—especially those with wounds and blockages in their legs—open bypass might still be the better option. A recent large trial called BEST-CLI confirmed that, in some cases, bypasses actually perform better. So we’re recalibrating.
Is open bypass becoming a lost art?
In some ways, yes. A lot of trainees coming out of fellowship in the past five years haven’t done that many bypasses. As endovascular options have improved, there are fewer patients who need bypasses. But bypass is still a very good operation—it works—and we don’t want to lose that skill. It might become a more specialized set of techniques reserved for larger centers.
What makes the work happening here stand out in vascular surgery?
From an aortic surgery standpoint, we’re by far the busiest complex aortic center in the city and the region. We do more branched and fenestrated cases than anyone, and we perform a much broader range of aortic surgeries—both endovascular and open—than most other places.
Part of that is simply because it’s what we do, it’s what we like to do, and we’re good at it. But what really makes Columbia unique is our collaboration with cardiac surgery. We work very closely with Dr. Hiroo Takayama and Dr. Amirali Masoumi. We discuss every patient together, and we scrub in together—whether it's an endovascular or an open repair. That kind of partnership isn’t common, and it lets us push the envelope in terms of what’s possible.
It allows us to treat essentially any part of the aorta—from the arch to thoracoabdominal aneurysms to complex dissections—using whatever approach is best. We also have a dedicated multidisciplinary aortic conference every week, where we go over cases, review imaging, and collaborate on decision-making. That team-based approach is a big part of what makes this program special.
Are there any new technologies you’re excited about?
One that’s pretty unique to us is a specialized polymer we inject into the aneurysm sac during endovascular repair. It’s a collection of tiny tubular devices—almost like soft, expandable pellets—that start in a compact form and then expand when they come into contact with blood or heat. We inject about a hundred of these into the aneurysm before removing the sheath.
They fill up the aneurysm sac, seal it off from any small vessels that might be leaking back in, and then trigger fibrosis, causing the aneurysm to shrink—sometimes it even disappears entirely. It helps the endograft seal more effectively and reduces the chance of complications.
We’ve done more of these procedures than anywhere else in the world, and there’s currently an ongoing multinational trial led by Dr. V. Patel. It’s a really promising innovation, and we’re proud to be leading in that space.
What about lower extremity procedures? What are you seeing on the horizon there?
We’re involved in a number of clinical trials, especially around new technologies for treating blockages in the legs. One of the most exciting is a bioresorbable scaffold—a next-generation device that’s kind of like a stent, but made from a polymer that dissolves over time. It props open the blood vessel and slowly releases a drug that prevents restenosis, or re-narrowing of the vessel. Then, over time, the scaffold is fully absorbed by the body.
That trial was recently published in the New England Journal of Medicine, and it was a big deal. Dr. Danielle Bajakian, one of my vascular colleagues, was one of the co-investigators, and Dr. Sahil Parikh from interventional cardiology was one of the PIs. It's an exciting development because it represents a step forward in treating chronic limb-threatening ischemia and peripheral artery disease (PAD) with long-term benefits and fewer permanent implants.
Are there other technologies you’re exploring in this space?
Yes—we’re also participating in trials that look at ways to measure blood flow in the legs non-invasively. These are especially important for PAD patients, where accurate, early assessment of limb perfusion can guide treatment decisions and help avoid unnecessary interventions. It's all part of a bigger push to treat PAD in a more effective, personalized, and patient-friendly way.
What’s important to know about Peripheral Arterial Disease (PAD) treatment?
PAD patients rarely have just one problem. It’s usually not just their legs. So the treatment has to be multidisciplinary—cardiology, endocrinology, podiatry, infectious disease, plastic surgery. You need a team. And these patients often become yours for life. That’s honestly one of the reasons I went into vascular surgery.
Screening seems like a key opportunity for earlier diagnosis. Are there steps being taken to improve access or education around it?
Yes, and it’s getting more focus now, but there are still major barriers. One of the biggest is reimbursement. For example, screening for PAD is really easy—it’s just a five-minute test using a blood pressure cuff on the ankle, called an ankle-brachial index. But it’s not reimbursed. So even though it’s simple and effective, primary care doctors are already overstretched and underpaid, and now you're asking them to do another test, for free, with no CPT code. Labs also aren’t going to want to take time away from reimbursable studies to do screenings that won’t be covered.
So right now, a lot of screening is happening on the volunteer or outreach level—health fairs, community events, things like that. But that’s not a long-term solution for large populations. It's a problem we’re actively trying to solve.
You’ve written about disparities in screening guidelines. Can you share more about that?
A lot of our current screening guidelines in vascular surgery are based on older randomized trials—and those trials mostly enrolled white men. That’s especially true for abdominal aortic aneurysm screening. Because women weren’t included in those studies, the U.S. Preventive Services Task Force doesn’t currently recommend screening for women, even if they smoke.
But women absolutely get aneurysms. Not as often as men, but still often enough that it matters—and it’s something other countries already account for. So we’ve been working to change that recommendation. It’s the same issue with PAD. There are lots of people who would benefit from screening, but without reimbursement and a formal recommendation, we’re not reaching them.
How are you preparing the next generation of vascular surgeons?
Simulation has become a huge part of training. Our fellows use high-end endovascular simulators. We co-run the Big Apple Bootcamp with Cornell every fall—it’s open to fellows from across the city. They practice leg procedures, endovascular repairs, you name it.
We also have cadaver labs, and industry has been a great partner—bringing in grafts, vein models, and other materials so residents can learn to do bypasses and anastomoses. We’ve also started recording our cases with a headlight camera and hope to build a video library for education.
Where do you see the field evolving in the next 5 to 10 years?
I think we’ll see more care organized around disease-specific teams, rather than individual specialties. Aortic surgery involves vascular, cardiac, cardiology, and genetics. PAD involves everything from podiatry to endocrinology. Same with vascular access. It’s becoming more multidisciplinary—and more organized that way.
We’re also expanding our footprint and doing more complex cases. I think we’ll continue to grow both locally and nationally in terms of prominence.
If you had no limits—no budget constraints, no red tape—what’s one thing you’d implement right now?
I’d upgrade our second hybrid room [a room that combines a traditional surgical operating space with advanced imaging capabilities associated with interventional procedures] and add real-shape sensing. It’s a fiber optic technology that allows you to do these procedures without radiation. The catheters and wires know where they are in space, so you don’t have to use fluoroscopy as much. It’d be a game changer—not just for the patient, but for everyone in the room.
Any final thoughts?
Just that these are lifelong diseases, our patients are ours for life. That’s what makes this work so meaningful. And it’s why I chose this field in the first place.
Related:
- Vascular Surgeon Draws on the Art of Surgery in His Own Way
- Predatory Artery Treatment for PAD: A Vascular Surgeon Weighs In
- A New Way of Approaching the Aorta: Bringing Cardiac and Vascular Surgeons Together